- Groundbreaking Results! Huang Zhifeng's Research Group of the School of Pharmaceutical Sciences at WMU Discovered a New Strategy for Sustained Antidiabetic Remission with Single Administration
- Author: Date:May 30, 2023

On May 10, Huang Zhifeng's research group of Academician Li Xiaokun's team at Wenzhou Medical University and Shen Wei's research group at ShanghaiTech University cooperated to publish important results online in Cell Metabolism (IF=31.37), a top international academic journal in the field of metabolism: "Sustained Remission of Type 2 Diabetes in Rodents by Centrally Administered Fibroblast Growth Factor 4". This study found that one intracerebroventricular administration or intranasal delivery of FGF4 in diabetic mice can induce a sustained antidiabetic effect of up to seven weeks, equivalent to several years in humans. Mechanism research showed that glucose-sensing neurons (GSNs) in the hypothalamus and their highly expressed FGFR1 are the cellular targets and biased receptor subtypes that mediate FGF4 and regulate persistent glucose homeostasis. This study has laid a key theoretical foundation for discovering new anti-diabetic targets and developing innovative drugs that can sustainably alleviate T2D from the perspective of central metabolic regulation.
Group leader of the research group drew an analogy with the relationship between the Buddhist monk Xuanzang and the Monkey King in Journey to the West to introduce the research results: the Monkey King (Glucose) is very skillful but is likely to make trouble (Diabetes) when overactive. Then Xuanzang (FGF4) will use the gold band (GSNs) to manage him and make him steady again (Homeostasis).
With the development of the social economy, diabetes has become a public health problem threatening global health. The latest national survey data show that the prevalence of diabetes among adults in China has reached 11.2%, with a total of nearly 160 million people. Type 2 diabetes (T2D) accounts for more than 90% of the large number of people with diabetes. At present, clinical treatment drugs for T2D mainly include insulin, biguanides, thiazolidinediones (TZDs), glucagon-like polypeptide 1 (GLP1) analogues, and dipeptidyl peptidase 4 (DPP4) inhibitors, etc., which cannot achieve long-term antidiabetic remission. As a result, most patients need long-term or even lifelong medication, which will lead to the gradual accumulation of side effects and a decrease in drug sensitivity and seriously endanger the physical and mental health and quality of life of patients. Therefore, it is of great scientific and clinical significance to explore new strategies for achieving sustained diabetic remission for patients with T2D on the basis of new mechanisms and targets.
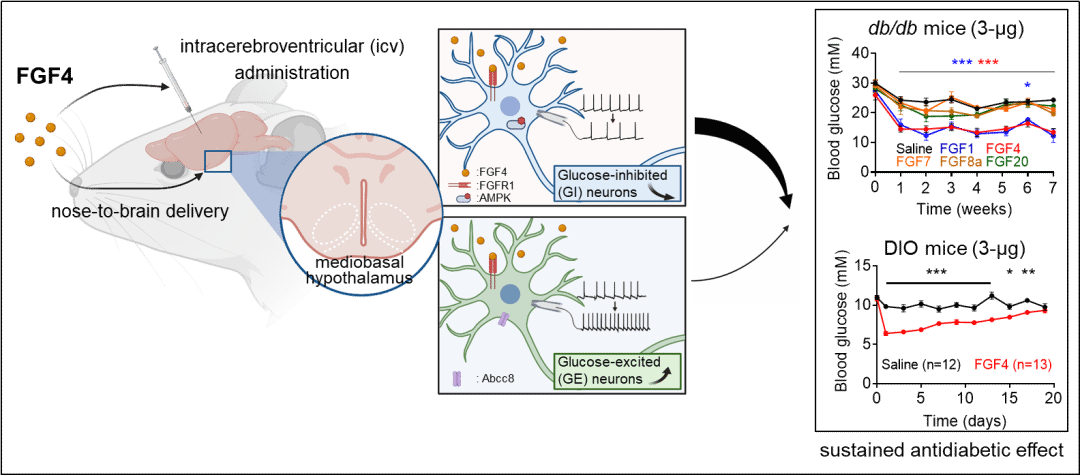
Mechanism diagrams of FGF4 exerting sustained antdiabetic effects through central nervous systems
As a secretory protein ligand, FGF binds to FGFR on the surface of the cell membrane to initiate specific signaling pathways, mediates cell fate trends, and affects multiple processes such as tissue regeneration and organism metabolism. Studies have shown that multiple members of the FGF family, such as FGF19, FGF21, and FGF1, can regulate glycolipid metabolism through peripheral administration. Additionally, related FGF signals can also regulate systemic energy metabolism by affecting the central nervous system, and inhibit the progression of T2D. Professor Huang Zhifeng's research group used the FGFR dimerization "threshold” model constructed in the previous stage (PNAS, 2020; Cell Rep, 2017), screened and identified FGF4 as a new candidate drug molecule (Nat Commun, 2021; Hepatology, 2022). Based on these previous findings, through joint efforts with Shen Wei's group and Zhang Jie's team of the Electrophysiology Laboratory at Chengdu Medical College, the research found that a single intracerebroventricular administration of FGF4 (icvFGF4) to T2D rodents could produce glucose control effects lasting more than seven weeks. Moreover, in the diet-induced obesity diabetes (DIO) model which is more similar to human metabolic syndrome, FGF4 exhibited a more prominent long-lasting hypoglycemic effect than other FGFs. The study implies the possibility of FGF4 as a potential candidate for sustained T2D control.
To further study the mechanism of persistent glucose control, the research team constructed a series of knockout mice and found that the hypothalamus, as an important part of the central nervous system that plays a key function in the regulation of metabolism, is also the main target of icvFGF4. Specifically, FGF4 targets the glucose-sensitive neurons (GSNs) in the mediobasal hypothalamus (MBH) and activates FGFR1c expressed in such neurons, thereby correcting the action potential frequency of GSNs in diabetic mice, restoring the percentage of GSNs, promoting glucose absorption in peripheral skeletal muscle across organs, and eliciting a sustained antidiabetic effect. At the end of this study, the research team designed a flexible nanoliposome loaded with FGF4 for intranasal administration, which also showed long-lasting antidiabetic effects, providing theoretical and technical support for the development of non-invasive therapy for diabetes.
Professor Huang Zhifeng of the School of Pharmaceutical Sciences at Wenzhou Medical University and Professor Shen Wei of the School of Life Science and Technology at ShanghaiTech University are co-corresponding authors of the paper. Sun Hongbin, Lin Wei, Tu Hongqing, and Tang Yu are co-first authors of the paper. Academician Li Xiaokun and Professor Moussa Mohammadi gave important guidance to this study. The relevant work was supported by the major research program of the National Natural Science Foundation of China, the National Key R&D Program of the Ministry of Science and Technology of the People's Republic of China, and the top-notch talent program of Oujiang Laboratory.
Article Link: https://www.cell.com/cell-metabolism/fulltext/S1550-4131(23)00172-9
The research also received comments from three well-known experts in related fields at home and abroad.
Song Baoliang (Academician of the Chinese Academy of Sciences, Vice President of Wuhan University, Executive Director of Chinese Society for Cell Biology)
Diabetes, characterized by hyperglycemia, has become a major health problem that endangers the health of the people in China and worldwide. In China, there are as much as 11.2% of adults who have diabetes. Conventional wisdom holds that peripheral metabolic organs such as the pancreas, liver, fat, and muscle were the core organs for the regulation of glucose homeostasis, while the nervous system might play a role in fine regulation. A variety of drugs used clinically for the treatment of diabetes, such as biguanides, sulfonylurea secretagogues, thiazolidinediones, and GLP1 receptor agonists, mainly target these peripheral metabolic tissues and organs. However, these drugs often only control blood glucose for a short period of time, and cannot help cure the disease through restoring glucose homeostasis for a long time. Therefore, discovering the mechanism of long-term glucose homeostasis regulation is a major challenge for basic research on diabetes.
In this work, two young professors in China worked closely together and found that a single FGF4 protein delivery can exert sustained anti-hyperglycemic effects through the hypothalamus for up to seven weeks. This discovery reveals the core role of the central nervous system in regulating blood glucose and is an excellent example of research on the role of the central nervous system in the regulation of glucose homeostasis. Professor Huang Zhifeng at Wenzhou Medical University focused on the physiological function of FGF, and Professor Shen Wei at ShanghaiTech University studied the role of the central nervous system in metabolic regulation. It was their cooperation that achieved the above innovative results. This work found that the centrally injected FGF4 protein exerts hypoglycemic effects through the FGFR1 expressed in the hypothalamus and glucose-sensitive neurons (GSNs). The findings provide molecular and cellular targets for targeting the hypothalamus and maintaining long-term blood glucose homeostasis, and also provide a scientific basis for the development of FGF4 into an innovative hypoglycemic drug at the source.
In addition, it is worth mentioning that although FGF4 significantly reduced the blood glucose level in T2D mice, it did not affect body weight and fat content remarkably. This also leads to a further question: how does the body coordinate the metabolic process of the three major sources of energy, namely glucose, fat and protein? In conclusion, this work identifies a novel long-acting glycemic factor FGF4, which provides a new strategy for the sustained treatment of metabolic diseases such as diabetes and advances our understanding of the mechanism of blood glucose regulation.
Xu Aimin (Chair Professor of School of Clinical Medicine, Director of State Key Laboratory of Pharmaceutical Biotechnology, The University of Hong Kong)
At present, there are more than 100 million diabetic patients in China, yet there is a lack of ideal and effective treatments (cures). It is usually impossible to achieve sustained remission of T2D unless a bariatric surgery is performed. Commonly used anti-diabetic drugs such as insulin, biguanides, glucagon-like peptide 1 (GLP1) analogues, dipeptidyl peptidyl peptidase-4 (DPP4) inhibitors only relieve symptoms, and patients need long-term or even lifelong medication. As a result, many patients become less sensitive to these drugs and adverse effects such as hypoglycemia and gastrointestinal problems are common.
In recent years, a number of studies have shown that multiple members of the FGF family (such as FGF19, FGF21, FGF1, and FGF4) have important glycolipid metabolism regulatory functions. Scarlet’s research team at the University of Washington found that a single intracerebroventricular administration of the paracrine FGF1 (icv) in db/db and ob/ob mouse models with genetically spontaneous type 2 diabetes could induce sustained diabetes remission for up to several weeks (Nat Med. 2016, 22 (7), 800-6). However, icvFGF1 is ineffective in the diet-induced obese (DIO) mouse model, and its mechanisms for sustained glucose control remain unclear. Academician Li Xiaokun and Professor Huang Zhifeng of WMU have been engaged in the research of FGF, and found that peripheral administration of FGF4 targets skeletal muscle to regulate blood glucose (Nat Commun. 2021, 12(1):7256.) Based on previous findings, the team collaborated with research teams at ShanghaiTech University and Chengdu Medical College and found that centrally administered FGF4 could exert remarkable anti-hyperglycemic effects in db/db and DIO mice. Further mechanistic studies showed that FGF4 mainly exerts a lasting anti-hyperglycemic effect by targeting glucose sensitive neurons (GSNs) in the hypothalamus, exciting glucose-excited neurons while inhibiting glucose-inhibited neurons, and restoring the percentage of GE/GI. It is particularly surprising that the research team has also developed a non-invasive nasal delivery technology to release FGF4, which provides a potential strategy for non-invasive and lasting therapy for diabetes in the future.
Cai Dongsheng (Professor, Department of Molecular Pharmacology, Albert Einstein College of Medicine, USA)
The hypothalamus is the core part of the central nervous system involved in the regulation of energy metabolism, and its dysfunction can lead to systemic metabolic disorders such as obesity and diabetes. Therefore, exploring new strategies for diabetes treatment by targeting hypothalamus has become a frontier hotspot in scientific research. In this work, Huang Zhifeng and Shen Wei's team found that a single intracerebroventricular or intranasal administration of FGF4 exerts a lasting glucose control effect in T2D rodents for more than seven weeks. Moreover, the research team found and confirmed that glucose sensitive neurons (GSNs) in the mediobasal hypothalamus (MBH) and FGFR1 expressed in GSNs are key targets for mediating FGF and persistent glucose control. MBH is an important metabolic regulatory hub including VMH and ARC. It consists of a series of neuronal subtypes and neural circuits involved in feeding and glucose regulation, such as POMC, AGRP, ESR1 and GSNs. In this paper, the research team intervened these neuronal subtypes respectively and confirmed that GSNs are key targets of FGF4 to regulate glucose metabolism. With patch-clamp technology, the research also found that FGF could significantly increase the action potential frequency of GE and inhibit the activity of GI neurons. This work has effectively improved people's understanding of the relationship between FGF signaling and central metabolic regulation. However, due to the lack of specific CRE targeting GSNs, the physiological/pathological functions of the FGF4-FGFR1 signaling pathway in GSNs need further exploration.
Text translated by Zhang Na and reviewed by Sun You.
